Effect of Minimally Invasive Pain Intervention in Frozen Shoulder Patients: A Cross‑Sectional Study
- Type: Free
Anurag Agarwal, Shivani Rastogi, Sujeet Rai, Manoj Giri, Samiksha Parashar, Deepak Malviya, Deepti Sharma Department of Anesthesiology, CCM and Pain Medicine, Dr RMLIMS, Lucknow, Uttar Pradesh, India
Background: Adhesive capsulitis or frozen shoulder (FS) is the second most common disorder accounts for 15%–30% shoulder pain and functional disability. Suprascapular nerve (SSN) interventions with corticosteroid alone have shown limited duration efficacy, adding pulsed radiofrequency (PRF) provides long‑term relief. Aims and Objective: We aimed to analyze the efficacy of SSN intervention on pain relief and range of mobility in patients with FS. Settings and Design: This is a cross‑sectional study of 37 patients of FS who underwent SSN interventions in a dedicated pain medicine unit of the department of anesthesiology. Materials and Methods: Thirty‑seven patients, who underwent SSN interventions for FS and followed for 6 months, were included in this study. Pain (Visual Analog Scale [VAS]), range of motion (ROM) (17), and Oxford 12 point Shoulder Score (OSS) for functional outcomes were recorded. In the final analysis, two subsets of patients who underwent SSN steroid injection or SSN PRF plus steroid were found and compared using Student’s t‑test paired and independent with P < 0.05 considered significant at 95% confidence interval. Results: The patient population was demographically comparable. Mean VAS score and ROM improved at 1, 3, and 6 months to statistically significant. On comparing the subgroups, the VAS score and OSS in both the SI and PRF groups were significantly improved, but the PRF group showed highly significant improvement, showing better and sustained improvement in the PRF group. Conclusion: PRF with steroid injection of the SSN provides better and long‑lasting relief from pain and improved mobility in FS patients in comparison to steroid alone.
IntroductIon
Adhesive capsulitis commonly called frozen shoulder (FS) is the second most common musculoskeletal disorder in adults accounting for 15%–30% shoulder pain.[1] FS is a progressive shoulder disorder causing severe pain with loss of movement and functional disability. [2,3] In elderly patients with history of diabetes mellitus, arthritis, and degenerative disease, the disease is more pronounced resulting in chronic pain which is difficult to treat.[4] The treatment options vary from conservative medical treatment to minimally invasive interventional pain procedures to extensive shoulder surgery.[5‑7]
Shoulder joint is innervated by three nerves: suprascapular nerve (SSN), axillary nerve, and lateral pectoral nerve. SSN gives sensory supply to 70% of the shoulder joint, superior, and posterosuperior regions of the shoulder joint and capsule and the acromioclavicular joint.[5] In addition, it supplies motor branches to supraspinatus and infraspinatus muscles.[6] Thus,
treatment for patients with shoulder pain, in addition to medical treatment and physiotherapy.[7]
SSN interventions using local anesthetics and steroids have been successful in treating chronic shoulder pain from degenerative disorders and inflammatory diseases. [8,9] However, the effects of SSN intervention using corticosteroids alone have shown limited duration efficacy.[10]
The idea of pulsed radiofrequency (PRF) was spawned after a chance meeting in 1993, and the first PRF procedure, on
a lumbar dorsal root ganglion, took place on February 1,
1996.[11] Pulsed mode radiofrequency (PRF) lesioning is a nonneuroablative, i.e., neuromodulatory, method for pain relief without evidence of neural damage.[12‑14] Very few case studies have been reported for PRF neuromodulation to the SSN which support its long‑term efficacy in pain relief.[15,16] The rationale behind this cross‑sectional study is to analyze SSN minimally invasive pain intervention in patients of FS.
Aims and objectives
We aimed to analyze the efficacy of SSN interventions in patients with FS on pain relief (Visual Analog Score), range of motion (ROM), and functional improvement assessment using Oxford Shoulder Score (OSS).
MaterIals and Methods
Study design
This study was conducted at a tertiary care 1100‑bedded multispecialty teaching hospital. A cross‑sectional study was conducted in the pain medicine unit of the department of Anesthesiology. Before the start of the study, the ethical clearance was taken from the institutional ethics committee (IEC110/20), and after necessary modifications,
the sample size was calculated. The pain medicine operation theater data were searched and analyzed for all patients who underwent SSN intervention for chronic shoulder pain, from July 2017 to July 2019, for this study. Our study follows the Helsinki Declaration. Written informed consent was obtained from the study participants.
Inclusion criteria
Patients suffering from chronic shoulder pain, not responding to conservative treatment for more than 6 weeks, and undergoing SSN pain intervention were included in this study.
Exclusion criteria
Patients with pain due to secondary causes, for example, acute trauma, fractures, bony deformity, glenohumeral joint pathology, acromioclavicular joint pathology, and rotator cuff disorder, and patients with known contraindications for minimally invasive pain interventions, for example, bleeding disorder, infection, and chronic obstructive pulmonary disease, were excluded from this study. Patients with allergy to drugs, pregnant patients, and patients with known coagulopathy were also excluded. Patients who did not give consent were also excluded.
After following all inclusion and exclusion criteria, 37 patients were found to be eligible for the study and their data were used for final statistical analysis. Patients’ details were recorded including epidemiological parameters, clinical parameters, and preoperative pain by Visual Analog Scale (VAS), ROM[1,7] and Oxford 12‑point Shoulder Score (OSS)[.18] All patients included in the study were followed for 6 months. All patients were taken after written consent and preoperative workup.
In the final analysis, two subsets of patients who underwent either SSN steroid injection or SSN PRF treatment were compared.
Suprascapular nerve intervention technique
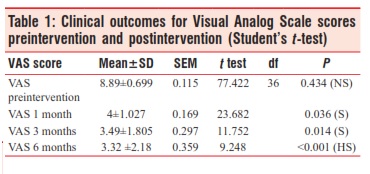
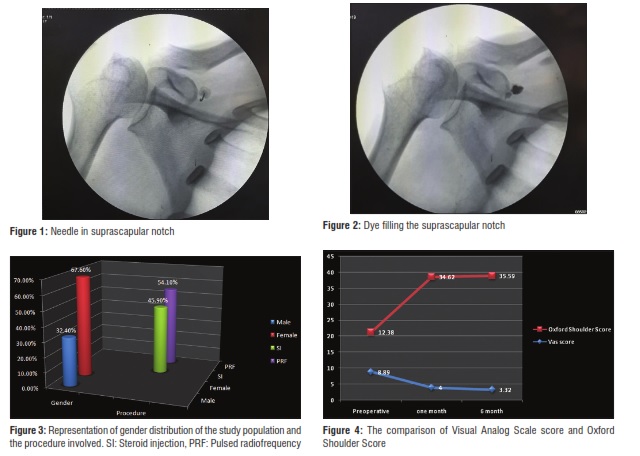
All cases were done with a patient in prone position with affected arm on the side of the patient. A C‑arm fluoroscope with 15°–20° cranial tilt and 10°–15° ipsilateral oblique tilt was used to visualize the suprascapular notch [Figures 1 and 2]. Then, a 22G, 10 cm RF cannulae (SMK RF Cannulae) was used to enter the suprascapular notch. Sensory stimulation at 50 Hz and motor stimulation at 2 Hz were used to localize the SSN. After negative aspiration, an injection of 8 ml of 0.25% bupivacaine plus 40 mg injection triamcinolone or a long duration pulsed radiofrequency treatment was done at 2 Hz with a maximum temperature of 42°C for 480 s was done[1.5,19] All patients were observed for 2 h and then discharged with instructions to do ROM exercises of the treated shoulder joint.
Data and statistical analysis
The internal consistency of any identified, and original, subscales was tested with Cronbach’s alpha. Alpha values in the range of 0.80–0.90 were considered optimal, with a minimum alpha of 0.70 being necessary to claim internal consistency. The standard error of mean was calculated as the standard deviation multiplied by the square root of one minus the intraclass correlation coefficient. Chi‑square test was utilized for demographic data, and both paired Student’s
t‑test and independent t‑test were used to compare pain scores in those with a good or poor recovery. The association between the change in pain VAS score and the Oxford Shoulder Score was quantified by the Spearman rank correlation coefficient (r). We determined test–retest reliability in those who had rated their pain state as unchanged or almost the same (global rating scores of 1, 0 or 1) using the intraclass correlation coefficient. A significant difference was accepted at P < 0.05. All statistical analyses were performed using Statistical Package for Social Sciences (SPSS)‑21, Chicago, Illinois, USA for data analysis. P < 0.05 considered with 95% confidence interval in the study.
results and observatIons
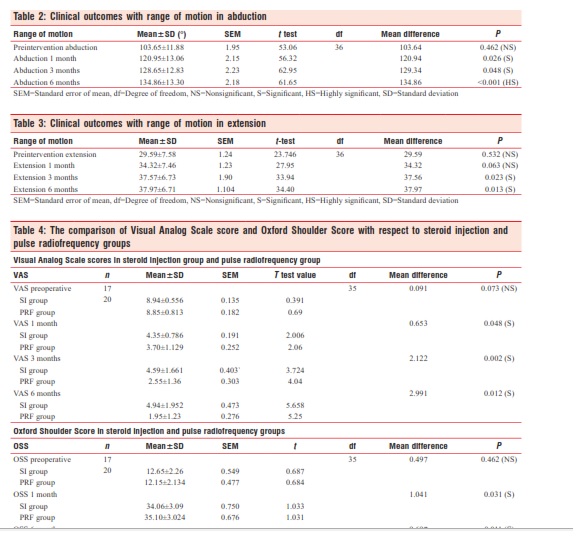
The demographic data of our patients’ population has shown homogeneity in both the subgroups. The mean age of our patients was 55 + 10.55 years. There was a female preponderance in our patient population (total patients 37, females 25 [67.6%] and males 12 [32.4%]). Seventeen (45.9%) out of 37 patients underwent steroid injection of SSN and 20 (54.1%) underwent PRF treatment in addition to steroid injection [Figure 3].c2 = 17.108; P = 0.705 Preintervention, the mean VAS score was 8.89 ± 0.699 (P =0.434), which improved at 1, 3, and 6 months to 4 ± 1.027 (P= 0.036), 3.49 ± 1.805 (P = 0.014), and 3.32 ± 2.18 (P = 0.0012), respectively, in all patients, which was statistically significant [Table 1]. Preintervention, ROM abduction and extension were 103.65° ± 11.88° and 29.59° ± 7.5°, respectively. Postintervention, abduction showed improvement at 1, 3, and 6 months to 120.95 ± 13.06 (P = 0.026), 128.65 ± 12.83 (P = 0.056), and 134.86 ± 13.30 (P = 0.001) and extension showed improvement at 3 and 6 months to 37.57 ± 6.37 (P = 0.023, S) and 37.97 ± 6.71 (P = 0.013, S), respectively, in all patients [Tables 2 and 3]. This shows that pain interventions are effective in improvement in ROM.
On comparison between the subgroups, the VAS score in the SI and PRF groups was significantly improved at 1 month (4.35 ± 0.786, P = 0.014 and 3.70 ± 1.129,
0.047); at 3 and 6 months, the PRF group showed highly significant (2.55 ± 1.36, P = 0.001 and 1.95 ± 1.23,P = 0.001) improvement in VAS scores while the SI group showed significant improvement (4.59 ± 1.66, P = 0.623 and 4.94 ± 1.952, P = 0.040), showing better and sustained
VAS=Visual Analog Scale, SEM=Standard error of mean, df=Degree of freedom, NS=Nonsignificant, S=Significant, HS=Highly significant, SD=Standard deviation
improvement in the PRF group. The preintervention Oxford Shoulder Score in the SI and PRF groups was 12.65 ± 2.26 and 12.15 ± 2.134, respectively, which improved to statistically significant values at 1 and 6 months 34.06 ± 3.09, P = 0.031, S and 30.35 ± 6.09, P = 0.011, S (SI group) and 35.10 ± 3.024 P = 0.021, S and 40.05 ± 4.96 P = 0.011, S (PRF group) [Table 4 and Figure 4], showing functional restoration in all patients who underwent pain interventions.
Inference
- Total population n (%) = 37 (100%)
- Total number of females = n 1 (%) = 25 (67.6%)
- Total number of males = n 2 (%) = 12 (32.4%).
Procedure
-
SI = 17 (45.9%)
-
PRF = 20 (54.1%).
dIscussIon
FS patients usually present in the sixth decade of life and onset before the age of 40 is very uncommon. The peak age is 56 years, and the condition occurs slightly more in women than men. The condition affects both sides equally, but nondominant shoulder is slightly more likely to be affected.
SEM=Standard error of mean, df=Degree of freedom, NS=Nonsignificant, S=Significant, HS=Highly significant, SI group=Steroid injection, PRF group=Pulse radiofrequency, SD=Standard deviation, OSS=Oxford 12‑point Shoulder Score
However, sequential bilateral occurrence may be found in up to 50% of patients.[20‑23]
Reeves[24] in a prospective study of 41 patients with 5–10‑year follow‑up found that only 39% of patients had full recovery. This long period of pain and disability deprives the patients of their routine activities of daily living and also poses occupational difficulties, thus adversely affecting their quality of life (QOL).FS can be classified either as primary (idiopathic) or secondary (associated with systemic diseases). The most common association is with diabetes mellitus, and the incidence is reported to be 10%–36%; [23] in these patients, it is often more severe and more resistant to treatment.[25] Other associated causes include thyroid disease, adrenal disease, cardiopulmonary disease, hyperlipidemia, and patients with stroke due to immobilization.[20]
The etiology of FS remains unclear. The disease process particularly affects the anterosuperior joint capsule and the coracohumeral ligament. [26] Bunker [27] studied histological samples of capsular tissue from patients with FS and found a pathological picture comparable to Dupuytren’s disease.
Management
The goal of treatment of FS is to restore the shoulder to a painless and functional joint. No definitive treatment strategy has been established, and many different management strategies are being used. Common conservative treatments include oral medication, physical therapy, exercise, steroid injection, and hydrodilatation.
Physiotherapy
Physiotherapy is widely accepted as an initial treatment in many shoulder conditions including FS. Physiotherapy forms the mainstay of early and mid‑stage disease. In general, physiotherapy is simultaneously combined with other treatment modalities as an adjunctive intervention; a Cochrane study concludes that there is little overall evidence to support physiotherapy alone in the treatment of FS[.28] Physical therapy can be combined with ultrasonic therapy, transcutaneous electrical nerve stimulation, shock‑wave therapy, low‑level laser therapy, hydrotherapy, and minimally invasive pain interventions as SSN PRF.
Pharmacological therapy, including NSAIDs and systemic or intra‑articular corticosteroids, provides symptomatic management and serves as an adjunct to physical therapy. Pain management is a key feature as it allows patients to tolerate physical therapy to improve ROM. NSAIDs are generally recommended for short‑term pain relief. The role of oral corticosteroids has been examined in multiple studies. Most of these demonstrate a short‑term benefit with a reduction in pain, especially during the early stages of FS.[29,30]
SSN minimally invasive percutaneous intervention with local anesthetic agent and small doses of steroids and PRF treatment are increasingly used in the multimodal treatment of FS. They are safe and well‑tolerated treatment option and effective in reducing pain severity and functional disability and hence improve QOL of the patients with FS. [31] Pulsed mode radiofrequency (PRF) lesioning is a nonneuroablative, i.e., neuromodulatory, method for pain relief, and can relieve pain without evidence of neural damage.
In patients with failed conservative care including poor response to minimally invasive pain interventions like SSN‑PRF, surgical interventions such as manipulation under anesthesia and arthroscopic capsular release under general anesthesia can be employed.
The aim of our retrospective study was to evaluate the use of minimally invasive and percutaneous pain interventions (SSN steroid injection and SSN PRF) in the management of FS.
Data from the pain medicine operation theater were taken out and analyzed from June 2017 to June 2019. Total 37 patients underwent minimally invasive pain intervention for FS during this period and were included in the final analysis. Our patient population shows female preponderance, similar to the studies by Neviaser and Neviaser,[19] Lloyd‑Roberts and French,[32] and Kothari et al.[33] Out of these 37 patients, 17 patients received steroid injection and 20 patients were given PRF with steroid.
The VAS pain score shows a statistically significant improvement from preoperative to 1 month (P = 0.036) and 3 months (P = 0.014) and a highly significant difference at 6 months (P = 0012) in all patients. On comparing the subgroups, the VAS improved to highly significant values at 6 months in the PRF group showing PRF to be better in pain relief in comparison to the steroid group [Table 2]. Shanahan et al. [2] and Shah and Racz[11,34] also concluded in their study that PRF lesioning of the SSN is effective for relieving various acute and chronic shoulder pain syndromes.
The clinical outcomes with ROM in abduction in our study showed a consistent and significant improvement at various time intervals and extension also showed a significant improvement at 3‑ and 6‑month duration in all patients. This suggests that there is a remarkable improvement in abduction ROM [Tables 2 and 3]. Our results were similar to studies done by Liliang et al., [3] and Snidvongs and Mehta [35] have also shown in their studies that PRF of SSN provides clinical improvement in FS patients.
The 12‑point Oxford Shoulder Score preintervention was statistically nonsignificant in both the groups. Postintervention, the OSS shows a significant improvement in the SI and PRF groups showing improvement in functional capacity and QOL which was more pronounced and long lasting in the PRF group. Jang et al. [6] also reported that PRF neuromodulation of the SSN is an effective treatment for chronic shoulder pain, and the effect was sustained over a relatively long period pain with improvement in OSS with an increase in functional capacity of patients.
conclusIon
This study highlights the growing importance of PRF procedure in chronic shoulder pain, especially in clinical scenarios where steroid injection procedure is not long lasting Agarwal, et al.: Suprascapular nerve intervention for frozen shoulder in pain relief, PRF added to significant improvement in range of shoulder motion, pain, and functional capacity than steroid alone injection procedure.
Thus, the study indicates that the application of PRF treatment with steroid injection of the SSN provides better and long‑lasting relief from pain and mobility in comparison to steroid injection alone.
Limitation
Our study has some limitations. First, although the VAS and mobility of the shoulder are proven tools for the quantification of pain, they are subjective outcome measures because they according to individual persons. Second, the small sample size limits the strength and generalizability of our observations.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards (in case humans are involved).
Key points (High light of article)
-
Shoulder pain treatment in frozen shoulder or adhesive capsulitis
-
Role of minimally invasive intervention in frozen shoulder use of steroid, physiotherapy, and pulsed radiofrequency
-
Role of radiofrequency in suprascapular nerve
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
references
- Pope DP, Croft PR, Pritchard CM, Silman Prevalence of shoulder
pain in the community: The influence of case definition. Ann Rheum Dis 1997;56:308‑12.
- Shanahan EM, Ahern M, Smith M, Wetherall M, Bresnihan B, FitzGerald O. Suprascapular nerve block (using bupivacaine and methylprednisolone acetate) in chronic shoulder Ann Rheum Dis 2003;62:400‑6.
- Liliang PC, Lu K, Liang CL, Tsai YD, Hsieh CH, Chen Pulsed radiofrequency lesioning of the suprascapular nerve for chronic shoulder pain: A preliminary report. Pain Med 2009;10:70‑5.
- Jones DF, Hodgden JD, Onarecker In adults with osteoarthritis of the knee, is conservative management more effective than intra‑articular corticosteroid injections in relieving pain? J Okla State Med Assoc 2018;111:712‑3.
- Ritchie ED, Tong D, Chung F, Norris AM, Miniaci A, Vairavanathan Suprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery: A new modality? Anesth Analg 1997;84:1306‑12.
- Jang JS, Choi HJ, Kang SH, Yang JS, Lee JJ, Hwang SM. Effect of pulsed radiofrequency neuromodulation on clinical improvements in the patients of chronic intractable shoulder pain. J Korean Neurosurg Soc 2013;54:507‑10.
- Jones DS, Chattopadhyay Suprascapular nerve block for the treatment of frozen shoulder in primary care: A randomized trial. Br J Gen Pract 1999;49:39‑41.
- Ozkan K, Ozcekic AN, Sarar S, Cift H, Ozkan FU, Unay K. Suprascapular nerve block for the treatment of frozen Saudi J Anaesth 2012;6:52‑5.
- Janda DH, Hawkins Shoulder manipulation in patients with adhesive capsulitis and diabetes mellitus: A clinical note. J Shoulder Elbow Surg 1993;2:36‑8.
- Shah RV, Racz GB. Pulsed mode radiofrequency lesioning of the suprascapular nerve for the treatment of chronic shoulder Pain Physician 2003;6:503‑6.
- Gurbet A, Türker G, Bozkurt M, Keskin E, Uçkunkaya N, Sahin S. [Efficacy of pulsed mode radiofrequency lesioning of the suprascapular nerve in chronic shoulder pain secondary to rotator cuff rupture]. Agri 2005;17:48‑52.
- Roach KE, Budiman‑Mak E, Songsiridej N, Lertratanakul Y. Development of a shoulder pain and disability Arthritis Care Res 1991;4:143‑9.
- Choi HJ, Choi SK, Kim TS, Lim YJ. Pulsed radiofrequency neuromodulation treatment on the lateral femoral cutaneous nerve for the treatment of meralgia J Korean Neurosurg Soc 2011;50:151‑3.
- Dahan TH, Fortin L, Pelletier M, Petit M, Vadeboncoeur R, Suissa S. Double blind randomized clinical trial examining the efficacy of bupivacaine suprascapular nerve blocks in frozen J Rheumatol 2000;27:1464‑9.
- Gado K, Emery Modified suprascapular nerve block with bupivacaine alone effectively controls chronic shoulder pain in patients with rheumatoid arthritis. Ann Rheum Dis 1993;52:215‑8.
- Green S, Buchbinder R, Glazier R, Forbes Systematic review of randomised controlled trials of interventions for painful shoulder: Selection criteria, outcome assessment, and efficacy. BMJ 1998;316:354‑60.
- Luleci N, Ozdemir U, Dere K, Toman H, Luleci E, Irban Evaluation of patients’ response to pulsed radiofrequency treatment applied to the suprascapular nerve in patients with chronic shoulder pain. J Back Musculoskelet Rehabil 2011;24:189‑94.
- Dawson J, Fitzpatrick R, Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br 1996;78:593‑600.
- Neviaser AS, Neviaser Adhesive capsulitis of the shoulder. J Am Acad Orthop Surg 2011;19:536‑42.
- Morén‑Hybbinette I, Moritz U, Scherstén The clinical picture of the painful diabetic shoulder‑natural history, social consequences and analysis of concomitant hand syndrome. Acta Med Scand 1987;221:73‑82.
- Pal B, Anderson J, Dick WC, Griffiths Limitation of joint mobility and shoulder capsulitis in insulin‑ and non‑insulin‑dependent diabetes mellitus. Br J Rheumatol 1986;25:147‑51.
- Sattar MA, Luqman WA. Periarthritis: Another duration‑related complication of diabetes Diabetes Care 1985;8:507‑10.
- Dias R, Cutts S, Massoud Frozen shoulder. BMJ 2005;331:1453‑6.
- Reeves The natural history of the frozen shoulder syndrome. Scand J Rheumatol 1975;4:193‑6.
- Griggs SM, Ahn A, Green Idiopathic adhesive capsulitis. A prospective functional outcome study of nonoperative treatment. J Bone Joint Surg Am 2000;82:1398‑407.
- Ozaki J, Nakagawa Y, Sakurai G, Tamai Recalcitrant chronic adhesive capsulitis of the shoulder. Role of contracture of the coracohumeral ligament and rotator interval in pathogenesis and treatment. J Bone Joint Surg Am 1989;71:1511‑5.
- Bunker Frozen shoulder: Unravelling the enigma. Ann R Coll Surg Engl 1997;79:210‑3.
- Green S, Buchbinder R, Hetrick Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev 2003;(2):CD004258.
- Blockey NJ, Wright JK, Kellgren Oral cortisone therapy in periarthritis of the shoulder; a controlled trial. Br Med J 1954;1:1455‑7.
- Binder AI, Bulgen DY, Hazleman BL, Tudor J, Wraight P. Frozen shoulder: An arthrographic and radionuclear scan Ann Rheum Dis 1984;43:365‑9.
- Klç Z, Filiz MB, Çakr T, Toraman Addition of Suprascapular Nerve Block to a Physical Therapy Program Produces an Extra Benefit to Adhesive Capsulitis: A Randomized Controlled Trial. Am J Phys Med Rehabil 2015;94:912‑20.
- Lloyd‑Roberts GC, French Periarthritis of the shoulder: A study of the disease and its treatment. Br Med J 1959;1:1569‑71.
- Kothari SY, Srikumar V, Singh N. Comparative Efficacy of Platelet Rich Plasma Injection, Corticosteroid Injection and Ultrasonic Therapy in the Treatment of Periarthritis Shoulder. J Clin Diagn Res 2017;11:RC15‑8.
- Chua NH, Vissers KC, Sluijter Pulsed radiofrequency treatment in interventional pain management: Mechanisms and potential indications‑a review. Acta Neurochir (Wien) 2011;153:763‑71.
- Snidvongs S, Mehta Pulsed radio frequency: A non‑neurodestructive therapy in pain management. Curr Opin Support Palliat Care 2010;4:107‑10.
 Tecar
Tecar Shock Wave
Shock Wave Plasma
Plasma Laser
Laser Nikola
Nikola Kayser
Kayser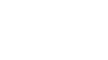 Fusion
Fusion





