The effect of laser therapy on plantar fasciitis
- Type: Free
Clinical efficacy of low-level laser therapy in plantar fasciitis , A systematic review and meta-analysis
Wei Wang, MSca, Weifeng Jiang, MScb, Chuanxi Tang, MDc, Xiao Zhang, MSca, Jie Xiang, MDa,∗
Abstract
Background: Emerging evidence suggests that low-level laser therapy (LLLT) for plantar fasciitis (PF) may be beneficial. However,
The convincing study investigating its effectiveness for treatment of PF was scarce. Therefore, a systematic review and meta-analysis was conducted to assess whether LLLT significantly relieve pain of patients with PF.
Methods: PubMed, EMBASE, EBSCO, Web of Science, China Biological Medicine Database, China National Knowledge
Infrastructure, Chinese Wan fang, and Cochrane CENTRAL were searched systematically up to March 2018.
Results: A total of 6 randomized controlled trials were included. The meta-analysis indicated that compared with control group, visual analogue scale (VAS) score significantly decreased at the end point of the treatment in LLLT group. In addition, this improvement is continued for up to 3 months. However, no significant difference was observed according to the Foot Function Index- pain subscale (FFI-p).
Conclusion: This meta-analysis indicates that the LLLT in patients with PF significantly relieves the heel pain and the excellent efficacy lasts for 3 months after treatment.
Abbreviations: AOFAS-F = function subscale of American Orthopedic Foot and Ankle Society Score, BMI = body mass index, CI
= confidence interval, ESWT = extracorporeal shock wave therapy, FFI-p = Foot Function Index-pain subscale, LLLT = low-level laser therapy, PF = plantar fasciitis, PRISMA = Preferred Reporting Items for Systematic Review and Meta-Analyses, RCTs = randomized controlled trials, SMD = standard mean difference, VAS = visual analogue scale.
Keywords: low-level laser therapy, meta-analysis, pain, plantar fasciitis
responses played a vital role in the pathological process.[1,8] Rather, emerging studies suggest that it is a degenerative process.[9] Nowadays, there are different invasive and noninvasive management strategies for PF, including nonsteroidal antiinflam matory drugs, oral analgesics, physical therapy, stretch exercise, foot orthotics, corticosteroid injection, platelet-rich plasma injection and botulinum toxin injection.[10–13] Although numerous studies reported that corticosteroid injection, as one of the most popular treatment for PF, may be effective to relieve pain in a short period of time,[14,15] it may lead to serious adverse events Such as PF rupture.[16] Low-level laser therapy (LLLT) is based on the principles of photochemistry that militates via photochemical or no thermal effects on cells.[17] Considerable studies have reported that LLLT could cure a variety of diseases, including sub acromial impingement syndrome,[18] acute and chronic pain,[19] stroke,[20] temporomandibular disorder,[21] oral mucositis,[22] lymphedema,[23] and carpal tunnel syndrome.[24] In recent years, LLLT has been used to relieve pain caused by PF.[25] Cinar et al reported that LLLT could significantly increase function subscale of American Orthopedic Foot and Ankle Society Score total score at 3 weeks and effectively improve walking distance and walking surface.[26] Additionally, ultrasound imaging results suggested that after LLLT intervention, plantar fascia thickness was significantly decreased when compared with that in the placebo group.[27] In 2017, a systematic review of laser therapy about PF was reported.[28] However, only 2 trials were included due to the limited documents. In this context, the purpose of this systematic review is to conduct an update and evaluate the usefulness and safety of LLLT in the treatment of PF.
-
Materials and methods
2.1. Search strategy
The study was conducted in accordance with guidelines from the Preferred Reporting Items for Systematic Reviews and Meta- analysis group (PRISMA).[29] Ethical approval was not necessary because all analyses were based on previous published studies. The electronic databases including PubMed, EMBASE, EBSCO, Web of Science, China Biological Medicine Database, China National Knowledge Infrastructure, Chinese Wanfang and Cochrane CENTRAL were systematically searched for the literatures between the establishment date and March 2018. The following search terms were used: plantar fasciitis (PF), plantar fasciopathy, and laser. In addition, the reference lists of the resulting publications and reviews were also searched for relevant literature. The literature search was limited to English and Chinese publications.
2.2. Selection criteria
The studies were selected according to the inclusion criteria: adult patients who were diagnosed with plantar heel pain or PF; experimental groups accepted LLLT alone or LLLT combined with other interventions; control groups accepted placebo or other interventions; reported data on at least 1 pain score, such as VAS; English or Chinese language publications; and randomized controlled trial (RCT). The exclusion criteria were as follows: no pain score was reported; not RCT; reviews, case report, abstract or animal studies; and duplicated data.
2.3. Data extraction
Data extraction was independently extracted by 2 authors, and disagreements were resolved by the third author. The extracted data included name of the first author, publication year, country, Study sample size, patient characteristics, treatment modality, follow-up duration, and outcomes.
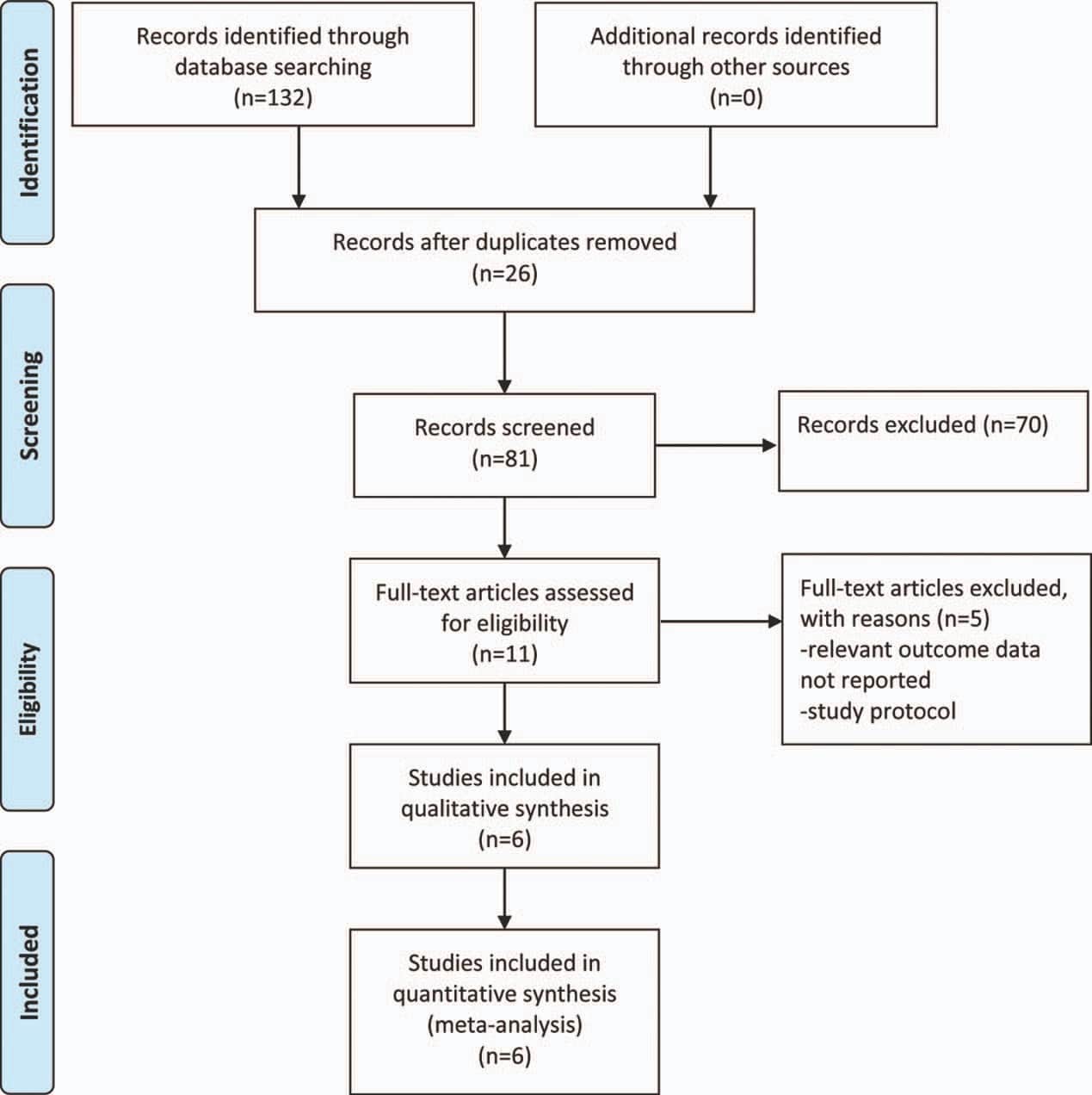
Figure 1. Flow diagram of included studies.
2.4. Risk of bias assessment
The Cochrane Collaboration risk of bias tool was used to assess the quality of RCT. All included studies were assessed in 6 domains: random sequence generation, allocation concealment,blinding of investigators and participants, blinding of outcomeassessment, incomplete of outcome data, selective reporting and other bias. Each domain has the low, unclear, or high risk.[30]
2.5. Statistical analysis
Statistical analysis was performed using RevMan 5.3 (The Cochrane Collaboration, Software Update, Oxford, UK) and Stata 12.0 (StataCorp, College Station, TX). For all, continuous outcomes were expressed as standard mean differences (SMDs) with 95% confidence intervals (95%CIs). A P-value of <.05 was considered to be statistically significant. Chi-squared test and I 2 statistic test values were calculated to test the heterogeneity across studies. An I value ≥50% or chi-squared value <0.05 was considered significant heterogeneity. A random effects model was 2 adopted when significant statistical heterogeneity was identified.
Otherwise, the fixed effects model was used. Sensitivity analysis was performed to detect the influence of a single study on the overall estimate via omitting 1 study in turn when necessary. Publication bias was assessed through Begg and Egger tests.
-
Results
3.1. Search results
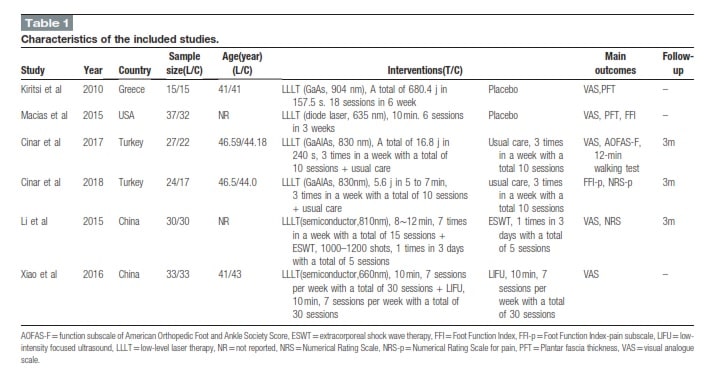
The initial literature search identified 132 studies, from which 26 studies were excluded due to the duplication. According to the inclusion and exclusion criteria, 6 RCTs[26,27,31–34] were finally included in this meta-analysis (Fig. 1). Two articles[33,34] were were in English. The characteristics of the included trials are provided in Table 1. Of the 6 RCTs, 2 studies published in Chinese, and 4 [26,27,31,32] compared LLLT with placebo, 1 article [27,31] [34] compared LLLT plus low-intensity focused ultrasound with low-intensity focused ultrasound, 1 trial [33] described LLLT plus extracorporeal shock wave therapy (ESWT) versus ESWT, and 2 trials [26,32] compared a combination of LLLT and a usual care with usual care alone.
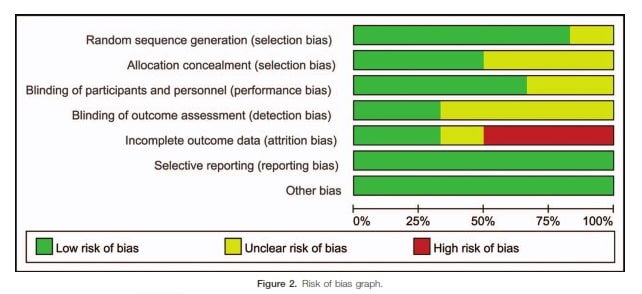
3.2. Methodological quality
Although all included studies claimed randomization, only 5 studies used the method of random sequences genera- tion.[26,27,31,32,34] Only 3 studies performed allocation proce- dure.[26,27,32] Four studies reported the blinding of participants and personnel.[26,27,31,32] And, 2 studies claimed the blinding of outcome assessors.[27,31] Three studies reported the incomplete outcome data.[26,27,32] The quality of these included studies is displayed in Figure 2.
3.3. Meta-analysis
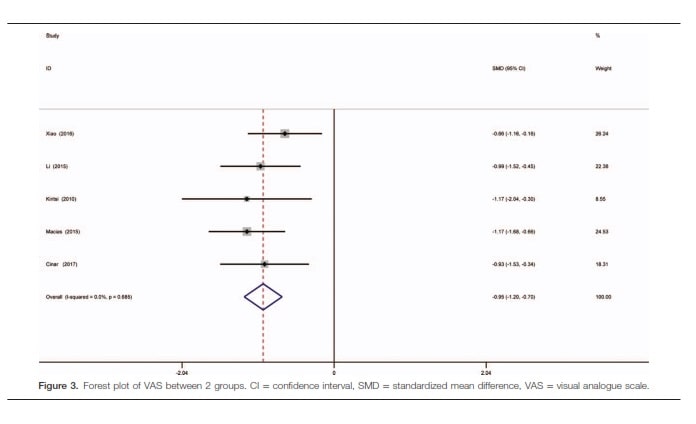
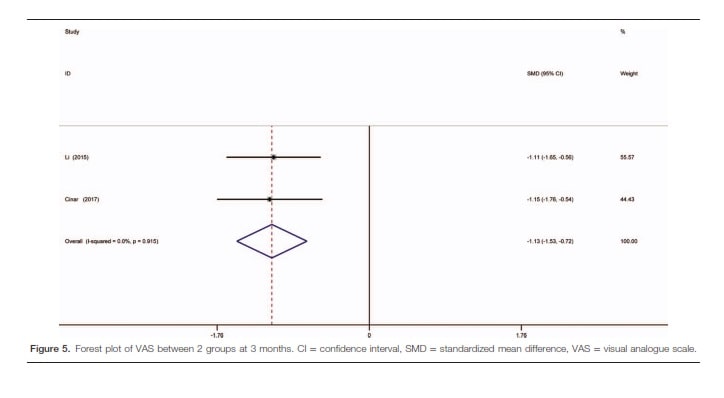
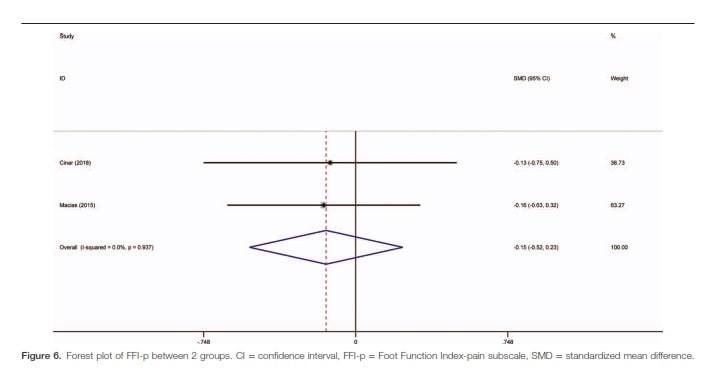
3.3.1. VAS score. The present meta-analysis is based on VAS and FFI-p scales. A total of 5 studies[26,27,31,33,34] with 274 patients provided analyzable data about VAS between LLLT group and control group. The meta-analysis demonstrated that VAS score was significantly reduced in the LLLT group (SMD =0.95; 95% CI 1.20 to 0.70; P<.001) (Fig. 3). Begg test (P=.642) and Egger test (P=.504) indicated no significant publication bias (Fig. 4). Additionally, compared with control group, VAS score was better in LLLT group at 3-month follow- up (SMD = 1.13; 95% CI 1.53 to 0.72; P<.001) (Fig. 5). 3.3.2. FFI-p score. Two studies [31,32]with 110 patients reported the FFI-p. Results indicated that no significant difference was found in the FFI-p (SMD = 0.15; 95% CI 0.52 to 0.23; P=.449) (Fig. 6). Besides, absence of adverse effects was found in 6 studies. The results are consistent with previous data that Showed laser therapy is safe, well tolerated, and less painful for the patients.
Discussion
In this study, a systematic review and meta-analysis was conducted to evaluate the effect of LLLT treatment of PF. Overall, the analysis suggested that LLLT can significantly relieve pain of PF for 3 months after treatment. The results of our review are consistent with the findings of previous studies, suggesting benefits of LLLT in heel pain caused by PF.[28] Our meta-analysis showed that LLLT intervention indeed alleviated pain as indicated by the decreased VAS score. In addition, compared with the baseline values, the VAS score was also significantly decreased at the period of 3-month follow-up after LLLT.
Despite LLLT have many applications in clinic, the exact mechanisms accounting for LLLT-mediated pain relief have not been identified. And some previous studies described a series of mechanisms as follows: peripheral neural blockade, enhancement of peripheral endogenous opioids, suppression of central synaptic activity, inhibition of histamine release, modulation of neuro- transmitters, promotion of adenosine triphosphate (ATP) production, reduction of muscle spasm, and increased production of antiinflammatory cytokines.[35–39] It is reported that there are several controversial cases about the LLLT treatment for PF, which might be due to the

the treatment protocols and types of LLLT. In general, 2 types of laser are used for PF: He-Ne laser and GaAlAs/GaAs laser. A prospective study showed that GaAlAs laser can significantly improve the pain of PF.[25] However, Macias et al[31] reported that pain attenuation was not obvious under the same treatment protocol. Compared with He-Ne laser, the efficacy of GaAlAs/ GaAs laser was performed better with deeper penetration. Several studies showed that patients suffering from PF could benefit from the GaAlAs/GaAs.[26,27,40] Conversely, Basford et al[41] reported that the application of GaAlAs could not improve the pain of PF. The inconsistencies in the efficacy of GaAlAs/GaAs laser may result from different doses. Basford et al[41] reported that their
treatment protocol was 1 J to the calcaneal origin and 2 J to the over the fascial arc, which is less than LLLT treatment PF recommended as treatment dose of a minimum of 8 J. In contrast, Ulusoy et al[40] applied LLLT at 8 J to the medial calcaneal area and the myofascial junction. Kiritsi et al[27] applied at 8.4J to the tendon insertion and the medial side of the fascia. As the therapeutic application of LLLT involves multiple variables, such as dose, locations, and frequency, it is unclear that which one is the optimum protocol. Therefore, future research should focus on exploring optimal treatment parameters to improve its treatment clinical efficacy.
This meta-analysis has some limitations. First, only 6 studies were included, and sample size was relatively small. Second, this meta-analysis lacks sufficient evidence to analyze the underlying influence factors (such as body mass index (BMI)) that may influence the effect of LLLT treatment. Third, the included studies lack sufficient data regarding longer-term outcomes of LLLT. Therefore, this study is only relevant short-term (up to 3 months) comparison data. Finally, the outcome just was obtained based on VAS, and other objective index (such as heel tenderness index and PF thickness) was not universally used in all included studies. Despite these limitations, the present meta-analysis still provided important clinical treatment information.
In conclusion, this meta-analysis demonstrated that LLLT may effectively relieve the heel pain of patients with PF, at least in the short term (i.e. 3 months). However, more large-scale, well- designed studies are needed urgently to further clarify long-term efficacy and optimal treatment parameters of LLLT.
Acknowledgments
We would like to thank all the authors in particular.
Author contributions
Conceptualization: Wei Wang, Jie Xiang, Weifeng Jiang.
Data curation: Wei Wang, Weifeng Jiang, Chuanxi Tang, Xiao Zhang.
Formal analysis: Wei Wang, Weifeng Jiang, Chuanxi Tang Investigation: Wei Wang, Jie Xiang, Xiao Zhang. Methodology: Wei Wang, Jie Xiang, Weifeng Jiang, Chuanxi
Tang.
Supervision: Wei Wang, Jie Xiang.
Validation: Weifeng Jiang, Chuanxi Tang, Xiao Zhang.
Visualization: Wei Wang, Jie Xiang.
Visualization: Wei Wang, Jie Xiang.
Writing – original draft: Wei Wang, Weifeng Jiang.
Writing – review and editing: Wei Wang, Weifeng Jiang, Chuanxi Tang.
References
[1] Beeson P. Plantar fasciopathy: revisiting the risk factors. J Foot Ankle Surg 2014;20:160–5.
[2] Rosenbaum AJ, DiPreta JA, Misener D. Plantar heel pain. Med Clin North Am 2014;98:339–52.
[3] Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med 2004;350:2159–66.
[4] Tahririan MA, Motififard M, Tahmasebi MN, et al. Plantar fasciitis. J Res Med Sci 2012;17:799–804.
[5] Orchard J. Plantar fasciitis. BMJ 2012;345:e6603.
[6] Barrett SJ, O’Malley R. Plantar fasciitis and other causes of heel pain. Am Fam Phys 1999;59:2200–6.
[7] Bolgla LA, Malone TR. Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice. J Athl Train 2004;39:77–82.
[8] Schwartz EN, Su J. Plantar fasciitis: a concise review. Perm J 2014;18: e105–7.
[9] Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc 2003;93:234–7.
[10] Crawford F, Thomson C. Interventions for treating plantar heel pain. Cochrane Database Syst Rev 2003;(3):CD000416.
[11] Rastegar S, Baradaran Mahdavi S, Hoseinzadeh B, et al. Comparison of dry needling and steroid injection in the treatment of plantar fasciitis: a single-blind randomized clinical trial. Int Orthop 2018;42:109–16.
[12] Singh P, Madanipour S, Bhamra JS, et al. A systematic review and meta- analysis of platelet-rich plasma versus corticosteroid injections for plantar fasciopathy. Int Orthop 2017;41:1169–81.
[13] Yang WY, Han YH, Cao XW, et al. Platelet-rich plasma as a treatment for plantar fasciitis: a meta-analysis of randomized controlled trials. Medicine (Baltimore) 2017;96:e8475.
[14] Schulhofer SD. Short-term benefits of ultrasound-guided corticosteroid injection in plantar fasciitis. Clin J Sport Med 2013;23:83–4.
[15] Chen CM, Lee M, Lin CH, et al. Comparative efficacy of corticosteroid injection and non-invasive treatments for plantar fasciitis: a systematic review and meta-analysis. Sci Rep 2018;8:4033.
[16] Landorf KB, Menz HB. Plantar heel pain and fasciitis. BMJ Clin Evid 2008;2008:
[17] de Castro JF, Abreu EG, Correia AV, et al. Low-level laser in prevention and treatment of oral mucositis in pediatric patients with acute lymphoblastic leukemia. Photomed Laser Surg 2013;31:613–8.
[18] Yeldan I, Cetin E, Ozdincler AR. The effectiveness of low-level laser therapy on shoulder function in subacromial impingement syndrome. Disabil Rehabil 2009;31:935–40.
[19] Chow RT, Johnson MI, Lopes-Martins RA, et al. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet 2009;374:1897–908.
[20] das Neves MF, Dos Reis MC, de Andrade EA, et al. Effects of low-level laser therapy (LLLT 808 nm) on lower limb spastic muscle activity in chronic stroke patients. Lasers Med Sci 2016;31:1293–300.
[21] Marini I, Gatto MR, Bonetti GA. Effects of superpulsed low-level laser therapy on temporomandibular joint pain. Clin J Pain 2010;26:611–6.
[22] Campos L, Cruz EP, Pereira FS, et al. Comparative study among three different phototherapy protocols to treat chemotherapy-induced oral mucositis in hamsters. J Biophotonics 2016;9:1236–45.
[23] Carati CJ, Anderson SN, Gannon BJ, et al. Treatment of postmastectomy lymphedema with low-level laser therapy: a double blind, placebo- controlled trial. Cancer 2003;98:1114–22.
[24] Fusakul Y, Aranyavalai T, Saensri P, et al. Low-level laser therapy with a wrist splint to treat carpal tunnel syndrome: a double-blinded randomized controlled trial. Lasers Med Sci 2014;29:1279–87.
[25] Jastifer JR, Catena F, Doty JF, et al. Low-level laser therapy for the treatment of chronic plantar fasciitis: a prospective study. Foot Ankle Int 2014;35:566–71.
[26] Cinar E, Saxena S, Uygur F. Low-level laser therapy in the management of plantar fasciitis: a randomized controlled trial. Lasers Med Sci 2018;33:949–58.
[27] Kiritsi O, Tsitas K, Malliaropoulos N, et al. Ultrasonographic evaluation of plantar fasciitis after low-level laser therapy: results of a double-blind, randomized, placebo-controlled trial. Lasers Med Sci 2010;25:275–81.
[28] Salvioli S, Guidi M, Marcotulli G. The effectiveness of conservative, non- pharmacological treatment, of plantar heel pain: a systematic review with meta-analysis. Foot (Edinb) 2017;33:57–67.
[29] Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med
2009;6:e1000097.
[30] Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collabo- ration’s tool for assessing risk of bias in randomised trials. BMJ
2011;343:d5928.
[31] Macias DM, Coughlin MJ, Zang K, et al. Low-level laser therapy at 635 nm for treatment of chronic plantar fasciitis: a placebo-controlled, randomized study. J Foot Ankle Surg 2015;54:768–72.
[32] Cinar E, Saxena S, Uygur F. Combination therapy versus exercise and orthotic support in the management of pain in plantar fasciitis: a randomized controlled trial. Foot Ankle Int 2018;39:406–14.
[33] Li XH, Yu HP, Shao L. The clinical observation of semiconductor laser combined with extracorporeal for plantar fasciitis. Laser J 2015;36:41– 141.
[34] Xiao HY, Ge HX, Wang Y, et al. Effect of low-intensity focused ultrasound combined with semi-conductor laser in treatment of patients with plantar fasciiti. Acad J Chin PLA Postgrad Med Sch 2016;37:970–2.
[35] Funk JO, Kruse A, Neustock P, et al. Helium-neon laser irradiation induces effects on cytokine production at the protein and the mRNA level. Exp Dermatol 1993;2:75–83.
[36] Hagiwara S, Iwasaka H, Hasegawa A, et al. Pre-irradiation of blood by gallium aluminum arsenide (830 nm) low-level laser enhances peripheral endogenous opioid analgesia in rats. Anesth Analg 2008;107:1058–63.
[37] Honmura A, Ishii A, Yanase M, et al. Analgesic effect of Ga-Al-As diode laser irradiation on hyperalgesia in carrageenin-induced inflammation. Lasers Surg Med 1993;13:463–9.
[38] Rochkind S, Nissan M, Lubart R, et al. The in-vivo-nerve response to direct low-energy-laser irradiation. Acta Neurochir (Wien) 1988;94:74–7.
[39] Schindl A, Schindl M, Schon H, et al. Low-intensity laser irradiation improves skin circulation in patients with diabetic microangiopathy. Diabetes Care 1998;21:580–4.
[40] Ulusoy A, Cerrahoglu L, Orguc S. Magnetic resonance imaging and clinical outcomes of laser therapy, ultrasound therapy, and extracorpo- real shock wave therapy for treatment of plantar fasciitis: a randomized controlled trial. J Foot Ankle Surg 2017;56:762–7.
[41] Basford JR, Malanga GA, Krause DA, et al. A randomized controlled evaluation of low-intensity laser therapy: plantar fasciitis. Arch Phys Med Rehabil 1998;79:249–54.
 Tecar
Tecar Shock Wave
Shock Wave Plasma
Plasma Laser
Laser Tesla
Tesla Nikola
Nikola Kayser
Kayser Fusion
Fusion





