The effect of Shock wave on the treatment of Plantar Fasciitis
- Type: Free
Extracorporeal shock wave therapy is effective in treating chronic plantar fasciitis
A meta-analysis of RCTs
Jiale Sun, MDa, Fuqiang Gao, MDb, Yanhua Wang, MDc, Wei Sun, MDb,∗, Baoguo Jiang, MDc,∗, Zirong Li, MDb
Abstract
Background: Plantar fasciitis (PF) is the most common reason for heel pain. The efficacy of extracorporeal shock wave therapy
(ESWT) as an ideal alternative to conservative treatments and surgery is controversial, and almost all previous articles compared general ESWT with placebo without indicating the kind of shock wave. We undertook a meta-analysis to compare the efficacy of general ESWT, focused shock wave (FSW), and radial shock wave (RSW) with placebo, to assess their effectiveness in chronic PF.
Methods: The PubMed, Medline, EmBase, Web of Science, and Cochrane library databases were searched for studies comparing FSW or RSW therapy with placebo in chronic PF. Clinical outcomes included the odds ratios (ORs) of pain relief, pain reduction, and complications. Relevant data were analyzed using RevMan v5.3.
Results: Nine studies involving 935 patients were included. ESWT had higher improvement rates than the placebo group (OR 2.58,95% confidence interval [CI] 1.97–3.39, P<.00001). ESWT had markedly lower standardized mean difference than placebo, with heterogeneity observed (standardized mean difference 1.01, 95% CI 0.01 to 2.03, P=.05, I2 =96%, P<.00001). FSW and RSW therapies had greater therapeutic success in pain relief than the placebo group (OR 2.17, 95% CI 1.49–3.16, P<.0001; OR 4.63,
95% CI 1.30–16.46, P=.02), but significant heterogeneity was observed in RSW therapy versus placebo (I2 =81%, P=.005).
Conclusion: This meta-analysis suggested that FSW therapy can relieve pain in chronic PF as an ideal alternative option; meanwhile, no firm conclusions of general ESWT and RSW effectiveness can be drawn. Due to variations in the included studies, additional trials are needed to validate these conclusions.
Abbreviations: ESWT = Extracorporeal shock wave therapy, FSW = focused shock wave, ORs = odds ratios, PF = plantar fasciitis, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses, RCTs = randomized controlled trials, RSW = radial shock wave, SMD = standardized mean difference.
Keywords: Extracorporeal shock wave therapy, heel pain relief, meta-analysis
- Introduction
Plantar fasciitis (PF) is a foot disease, and the most common cause of heel pain, accounting for about 11% to 15% of clinical symptoms requiring treatment.[1] Although the suffix “ –itis ” implies an inflammatory condition, mounting evidence indicates that this foot disorder is associated with degenerative changes, and should be appropriately classified as a “Fasciosis” or “Fasciopathy.”[1,2] Patients with PF may experience the most serious heel pain with the first few steps in the morning or after a period of rest.[1,2] The treatment options for relieving PF symptoms include activity modification, plantar fascia stretch, ice massage, night splints, no steroidal anti-inflammatory drugs combined with other treatment modalities, local steroid injections, Extracorporeal Shockwave therapy, and surgery.[3] Approximately 10% of PF patients cannot be relieved by conservative therapy, whose long course is not satisfactory.[4] In addition, surgical treatment is considered the last intervention because of serious injury, risks, and postoperative complications. Extracorporeal shock wave therapy (ESWT) has been widely used as an alternative treatment option for PF for decades due to its noninvasive nature, fast recovery time, and convenience for daily life of patients.[5,6] The specific mechanisms of ESWT in treating musculoskeletal pain remain unclear; however, multiple studies have shown that it can destroy sensory unmyelinated nerve fibers, and stimulate neovascularization and collagen synthesis in degenerative tissues.[7] Recently, both focused shock wave (FSW) and radial shock wave (RSW) therapies were introduced as treatment options for PF. RSW dispersed from the applicator does not concentrate on the tissue compared with FSW.[8] Several studies have demonstrated the function of ESWT in relieving heel pain. However, there were positive and negative results. Furthermore, some previous meta-analyses compared ESWT and sham or other therapeutic methods, without distinguishing which ESWT type is effective. It is uncertain whether general ESWT, including FSW and RSW therapies, is effective in relieving plantar heel pain. Such debate may be further acknowledged by our meta-analysis combined with previous analysis, aiming at providing useful information on efficacy of ESWT for the treatment of chronic PF.
- Materials and methods
This meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta- Analyses (PRISMA) guidelines.[9] Ethical approval for this study was unnecessary, as a review of existing literature not involving the handling of individual patient data.
2.1. Date sources and study selection
The PubMed, Medline, EmBase, Web of Science, and Cochrane library databases were searched up to July 2016, for comparative studies involving shock wave in the management of pain relief from plantar fasciitis. The search terms were: “extracorporeal shock wave therapy” OR “focused extracorporeal shock wave therapy” OR “radial extracorporeal shock wave therapy” AND “plantar fasciitis” OR “plantar fasciopathy” OR “heel pain.” Then, the articles were searched by abstract and title. Publication language was limited to English. The reference lists of all eligible studies and relevant reviews were manually searched for any additional trials.
2.2. Inclusion criteria
Studies that met the following criteria were included in the current meta-analysis: investigations of patients suffering from heel pain and diagnosed with chronic plantar fasciitis; studies involving the comparison between ESWT without anesthesia and sham therapy as control; randomized controlled trials (RCT).
2.3. Data extraction and quality assessment
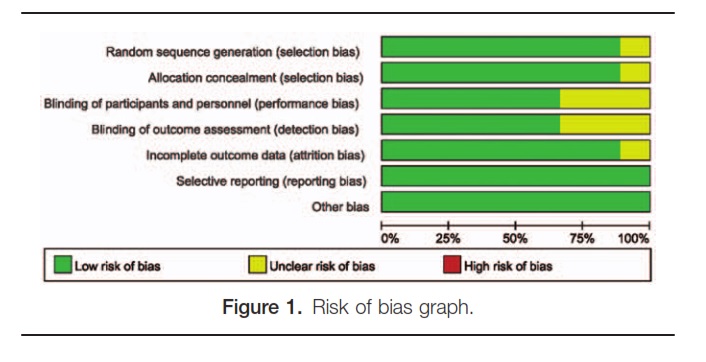
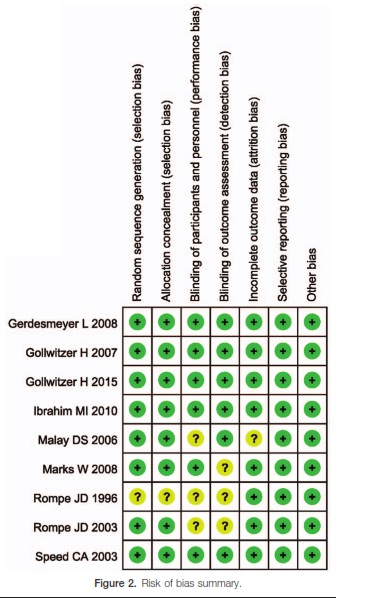
Data from the obtained articles were abstracted independently by 3 investigators (J.S., F.G., and W.Y.), including author’s name, year of publication, trial design, total participants and allocation, details of intervention (FSW or RSW, density of shock wave, and time of treatment) and control groups, and trial outcomes and results. Cochrane Risk of Bias Tool was used to assess the quality of clinical trials (Figs. 1 and 2). Discrepancy was resolved by discussing with other investigators and contacting the article’s authors if necessary.
2.4. Statistical analysis
Review Manager Software (Revman v5.3) was used to analyze experimental data from the included trials. Odds ratios (ORs) of successful treatments were assessed for dichotomous data. Heterogeneity among studies was estimated using the I2 statistics;
model was used when I2 <50%; otherwise, the random-effects model was adopted. P<.05 was considered statistically significant.
- Results
3.1. Study inclusion
The literature search identified a total of 326 articles, of which145 were considered to be relevant; 37 clinical RCTs were
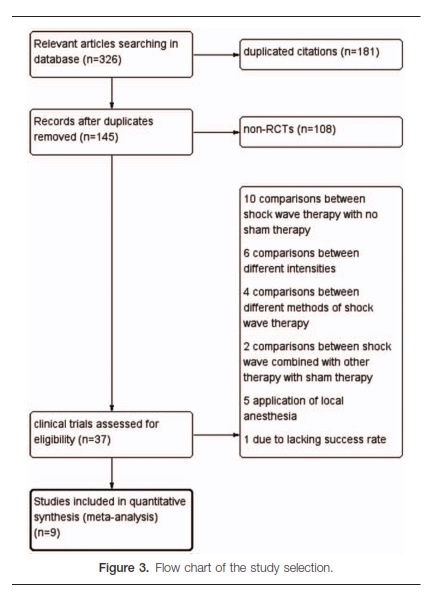
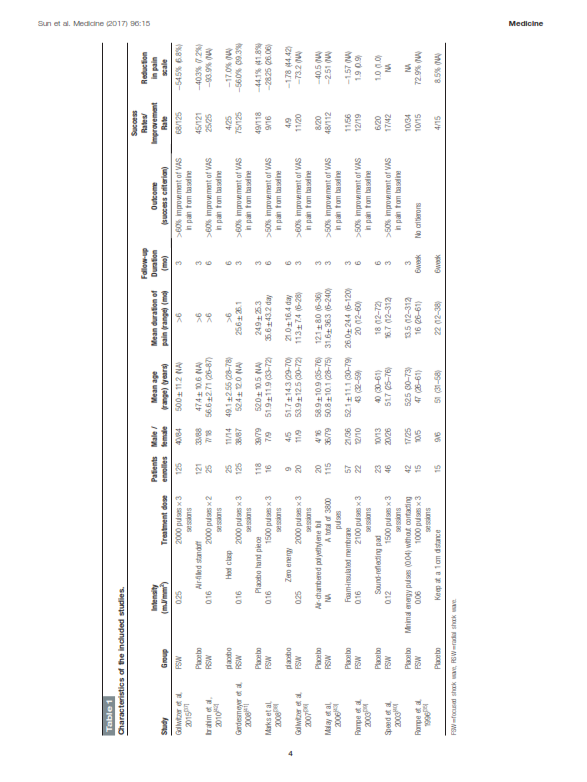
Screened. After assessing the abstracts and full text articles, 10 studies were excluded because of comparisons between focused or radial shock wave and other treatments rather than sham therapy;[10–19] 6 were excluded for comparisons between different intensities,[20–25] 2 for comparisons between shock wave therapy combined with other therapies and sham therapy,[26,27] 4 for comparisons between different methods of shock wave therapy,[28–31] 5 for applying local anesthesia totally,[5,6,32–34] and 1 for lacking the success rate.[8] Finally, 9 studies, including 6 reports comparing FSW therapy with a placebo,[35–40] and 3 comparing RSW,[41–43] were eligible for data extraction and meta-analysis based on inclusion and exclusion criteria. These articles involved 935 patients (Fig. 3) (Table 1).
3.2. Success or improvement rates
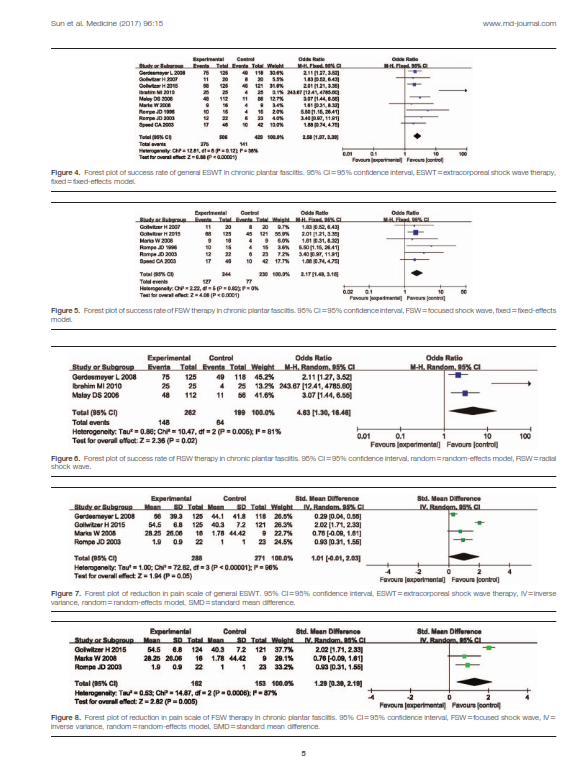
Therapeutic success was defined as a decrease in visual analogue scale (VAS) score from baseline larger than 50% or 60%, or VAS score of less than 4 cm after intervention, according to the included studies. In comparison, general ESWT had higher improvement or success rates than placebo as assessed by a fixed effects model (OR 2.58, 95% confidence interval [CI] 1.97–3.39, P< .00001, I 2 = 38%) (Fig. 4). According to the different shock wave types, a subgroup analysis of FSW and RSW therapies was performed. The FSW group involved 474 patients with 244 events, indicating that FSW therapy had greater improvement or success rates than placebo as assessed by a fixed-effects model (OR 2.17, 95% CI 1.49–3.16, P< .0001, I 2 = 0%) (Fig. 5). The RSW therapy group involved 461 patients with 262 events, suggesting that RSW therapy had higher pooled ORs (OR 4.63,95% CI 1.30–16.46, P=.02) than placebo, but significant heterogeneity was observed (I2 =81%, P=.005) (Fig. 6).
3.3. Reduction in pain scales
Only 4 trials provided adequate information regarding reduction in pain scale with standard error. Of these trials, 3 compared FSW therapy with placebo,[37–39] whereas 1 comparatively assessed RSW therapy and placebo.[41] Significant heterogeneity was observed in the comparisons of reduction in pain scale. General ESWT had greater reduction in pain scale than placebo (standardized mean difference [SMD] 1.01, 95% CI 0.01 to 2.03, P=.05) (Fig. 7), but 95% CI covered the value of 0, as analyzed by a random-effects model.
3.4. Complications
Seven of 9 included studies described complications of ESWT; there were no serious adverse events, such as hematomas, infections, and abnormal musculoskeletal events, recorded during patient follow-up. A few patients had feelings of discomfort, pain, swelling, and bruise during or after treatment, which may be considered intensity-related adverse events. These findings indicated that ESWT is a safe and effective treatment.
- Discussion
Unlike previously published meta-analyses that did not distinguish shock wave types, the current meta-analysis pooled comprehensive data on FSW and RSW therapies for chronic PF, and determine whether general ESWT, FSW therapy, and RSW therapy are effective treatments for chronic PF. In addition, few studies have compared the effects of FSW and RSW therapies, respectively, with those of placebo. In this meta- analysis, ESWT and RSW therapy for chronic PF might be more effective than placebo and FSW therapy, as safe alternative options.
General ESWT was shown to be effective and safe in the treatment of chronic PF in a comprehensive comparison of success or improvement rates including both shock wave types with controls. However, Speed et al[40] and Marks et al[38] found no significant difference between ESWT and sham therapy. General ESWT was probably more effective, according to the comparisons of pain scale reduction and significant heterogeneity that resulted in a wider range of SMD. Nevertheless, differences were observed in ESWT compared with sham therapy.
The FSW therapy is a traditional alternative option to operation, and was introduced in 1995. FSW devices generate energy focusing on a small region with the maximum energy level, which can penetrate some centimeters subcutaneously. [8] In the current meta-analysis, significant differences in success or improvement rates were observed in FSW therapy for chronic PF compared with sham therapy, and reduction in pain scale in FSW therapy (SMD 1.29,
[44–46] 2 = 87% in random-effects model) (Fig. 8) was higher than in the placebo groups. However, Speed et al found no significant difference between FSW and sham therapies. [40] [38] and Marks et al The RSW therapy is a relatively new method that was introduced in 2001. [8] Compared with FSW, RSW evices disperse the shock wave at the skin surface and distribute the energy radially into larger treatment tissue areas. Therefore, the
radial technique can be used to treat the painful region instead of a point, and an advantage of RSW therapy is extended treatment area.[8,41,43,47] We found that RSW therapy effectiveness may be due to significant heterogeneity; therefore, no solid conclusions can be drawn, although all included studies demonstrated the effectiveness of RSW therapy in chronic PF.
Most observed heterogeneity appeared to be attributed to clinical practice or trial’s methodology. First, in a comprehensive comparison of both shock wave types in reducing pain scale, variations of follow-up time in individual studies may have influenced the results. Gollwitzer et al[37] trail followed up for 3 months and the other trial for more than 6 months. Excluding Gollwitzer et al’s study revealed ESWT efficacy (SMD 0.57, 95% CI 0.12–1.01, P=.01) compared with placebo. Secondly, analyzing the success rates of RSW therapy and considering the far better effect in the study by Ibrahim et al,[42] we concluded that the high difference in participant numbers between the 3 trials evaluating RSW might have influenced the results. However, even excluding the Ibrahim et al’s trial, Gerdesmeyer et al[41] and Malay et al[43] still showed efficacy for RSW therapy (OR 2.39, 95% CI 1.57–3.65, P<.0001) compared with sham therapy. Thirdly, variations in success criteria in each study might have influenced the success rates. Malay et al[43] considered therapeutic success as a decrease of 50% or more in VAS score from baseline to the third visit, with a VAS score 4 cm; Gerdesmeyer et al[41] and Ibrahim et al[42] defined therapeutic success as a decrease in VAS score from baseline larger than 60%. By excluding Malay et al’s study, the efficacy of RSW therapy (OR 18.34, 95% CI 0.14–2413.75) compared with sham therapy remained, but heterogeneity was observed (I2 =90%, P=.001). Subgroup analysis based on participant numbers was not carried out due to insufficient data required for further confirmation.
The current meta-analysis included 9 studies not applying local anesthesia to most participations in the RCTs, because according to some literatures, application of local anesthesia would affect the efficacy of shock wave therapy.[30,48] Some previous meta- analyses did not take this into account. Meta-analyses by Yin et al,[49] Dizon et al,[50] and Zhiyun et al[51] did not exclude studies applying local anesthesia, and more inaccurate results may appear. Furthermore, almost all previous meta-analyses investigated common effectiveness of ESWT in chronic PF, not differentiating the shock wave type, lacking efficacy data about FSW or RSW compared with placebo, respectively. The studies by Yin et al[49]Aqil et al,[52] and many other studies compared ESWT (including FSW and RSW therapies) with placebo, which may make it difficult to accurately evaluate the efficacy of general ESWT for chronic PF if the 2 shock wave types have different effectiveness levels.
Numerous studies have evaluated the efficacy of FSW therapy, but yielded inconsistent results. Speed et al[40] and Marks et al[38] indicated that FSW has no significant treatment effect in patients, which appeared to be the placebo effect. However, Gollwitzer et al in 2007[36] and 2015,[37] respectively, enrolled 40 and 246 patients undergoing treatment with an intensity of 0.25mJ/mm2, and success rates in pain relief were 11/20 and 68/125, respectively, higher than with placebo therapy. In 2003, Rompe et al[39] enrolled 45 running athletes suffering from chronic PF and demonstrated the beneficial effects of FSW therapy. Therefore, FSW may be considered an effective and noninvasive treatment method. This meta-analysis suggests that FSW therapy should be recommended as remedial treatment after failure of traditional conservative therapy and before operation based on the different included studies. Moreover, the current meta-analysis compared FSW or RSW therapy with sham therapy, and different indicators to evaluate general ESWT effectiveness; due to significant heterogeneity, RSW therapy may probably have better effectiveness, and no firm conclusions that general ESWT (including FSW and RSW therapies) is effective could be drawn. In addition, we could not determine which shock wave type is more effective. There was only 1 study, the study by Lohrer et al,[8] comparing focused versus radial extracorporeal shock waves in plantar fasciitis, demonstrating the superiority of FSW therapy over RSW therapy. Due to the limited literature available on FSW versus RSW therapy, whether FSW is more effective than RSW remains to be studied. This meta-analysis had 4 limitations. First, we included only studies written in English, and some relevant studies in other languages may have been missed. Second, although we estimated the various articles based on inclusion and exclusion criteria, and also Cochrane Risk of Bias Tool, the sample sizes of several included studies were small, and a small proportion of the participants involved used local anesthesia because of unendurable pain rather than routine administration, which limited the statistical power of this meta-analysis. Third, some articles lacked data on functional recovery after shock wave therapy, and we could not estimate this parameter. Therefore, further assessment of comparative efficacy and functional recovery between FSW and RSW therapies is required. Fourth, more multicenter RCTs comparing FSW and RSW therapies are required to further confirm the comparative effectiveness of focused and radial shock wave therapies for treating chronic plantar fasciitis.
- Conclusions
Focused shock wave therapy appears to be associated with higher success rate and greater pain reduction compared with sham therapy in chronic plantar fasciitis patients. However, due to limitations of the included studies, more large-sample and high- quality clinical trials and systemic reviews are warranted to demonstrate the efficacy of general ESWT (including FSW and RSW therapies) and determine whether RSW therapy is an ideal alternative therapeutic method to conservative treatment and surgery.
References
[1] Rompe JD. Plantar fasciopathy. Sports Med Arthrosc 2009;17:100–4. [2] Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc
2003;93:234–7.
[3] Lim AT, How CH, Tan B. Management of plantar fasciitis in the outpatient setting. Singapore Med J 2016;57:168–70. quiz 171.
[4] Rompe JD, Furia J, Weil L, et al. Shock wave therapy for chronic plantar fasciopathy. Br Med Bull 2007;81-82:183–208.
[5] Theodore GH, Buch M, Amendola A, et al. Extracorporeal shock wave therapy for the treatment of plantar fasciitis. Foot Ankle Int 2004;25:
290–7.
[6] Ogden JA, Alvarez R, Levitt R, et al. Shock wave therapy for chronic proximal plantar fasciitis. Clin Orthop Relat Res 2001;47–59.
[7] Hsu RW, Hsu WH, Tai CL, et al. Effect of shock-wave therapy on patellar tendinopathy in a rabbit model. J Orthop Res 2004;22:221–7. [8] Lohrer H, Nauck T, Dorn-Lange NV, et al. Comparison of radial versus focused extracorporeal shock waves in plantar fasciitis using functional measures. Foot Ankle Int 2010;31:1–9.
[9] Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12.
[10] Eslamian F, Shakouri SK, Jahanjoo F, et al. Extra corporeal shock wave plantar fasciitis: a single blinded randomized clinical trial. Pain Med
2016;17:1722–31.
[11] Hammer DS, Adam F, Kreutz A, et al. Extracorporeal shock wave therapy (ESWT) in patients with chronic proximal plantar fasciitis: a 2- year follow-up. Foot Ankle Int 2003;24:823–8.
[12] Konjen N, Napnark T, Janchai S. A comparison of the effectiveness of radial extracorporeal shock wave therapy and ultrasound therapy in the treatment of chronic plantar fasciitis: a randomized controlled trial. J Med Assoc Thai 2015;98(suppl 1):S49–56.
[13] Mardani-Kivi M, Karimi Mobarakeh M, Hassanzadeh Z, et al.
Treatment outcomes of corticosteroid injection and extracorporeal shock wave therapy as two primary therapeutic methods for acute plantar fasciitis: a prospective randomized clinical trial. J Foot Ankle Surg 2015;54:1047–52.
[14] Porter MD, Shadbolt B. Intralesional corticosteroid injection versus extracorporeal shock wave therapy for plantar fasciopathy. Clin J Sport
Med 2005;15:119–24.
[15] Radwan YA, Mansour AM, Badawy WS. Resistant plantar fasciopathy: shock wave versus endoscopic plantar fascial release. Int Orthop 2012;36:2147–56.
[16] Roca B, Mendoza MA, Roca M. Comparison of extracorporeal shock wave therapy with botulinum toxin type A in the treatment of plantar fasciitis. Disabil Rehabil 2016;38:2114–21.
[17] Rompe JD, Cacchio A, Weil L, et al. Plantar fascia-specific stretching versus radial shock-wave therapy as initial treatment of plantar fasciopathy. J Bone Joint Surg Am 2010;92:2514–22.
[18] Rompe JD, Furia J, Cacchio A, et al. Radial shock wave treatment alone
is less efficient than radial shock wave treatment combined with tissue- specific plantar fascia-stretching in patients with chronic plantar heel pain. Int J Surg 2015;24:135–42.
[19] Wang CJ, Wang FS, Yang KD, et al. Long-term results of extracorporeal shockwave treatment for plantar fasciitis. Am J Sports Med 2006;34: 592–6.
[20] Buchbinder R, Ptasznik R, Gordon J, et al. Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: a randomized controlled trial. JAMA 2002;288:1364–72.
[21] Chow IH, Cheing GL. Comparison of different energy densities of extracorporeal shock wave therapy (ESWT) for the management of chronic heel pain. Clin Rehabil 2007;21:131–41.
[22] Lee SJ, Kang JH, Kim JY, et al. Dose-related effect of extracorporeal shock wave therapy for plantar fasciitis. Ann Rehabil Med 2013;37: 379–88.
[23] Liang HW, Wang TG, Chen WS, et al. Thinner plantar fascia predicts decreased pain after extracorporeal shock wave therapy. Clin Orthop Relat Res 2007;460:219–25.
[24] Park JW, Yoon K, Chun KS, et al. Long-term outcome of low-energy extracorporeal shock wave therapy for plantar fasciitis: comparative analysis according to ultrasonographic findings. Ann Rehabil Med 2014;38:534–40.
[25] Rompe JD, Schoellner C, Nafe B. Evaluation of low-energy extracorpo- real shock-wave application for treatment of chronic plantar fasciitis. J Bone Joint Surg Am 2002;84-A:335–41.
[26] Vahdatpour B, Sajadieh S, Bateni V, et al. Extracorporeal shock wave
therapy in patients with plantar fasciitis. A randomized, placebo- controlled trial with ultrasonographic and subjective outcome assess- ments. J Res Med Sci 2012;17:834–8.
[27] Yan W, Sun S, Li X. Therapeutic effect of extracorporeal shock wave combined with orthopaedic insole on plantar fasciitis. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2014;39:1326–30.
[28] Dorotka R, Sabeti M, Jimenez-Boj E, et al. Location modalities for focused extracorporeal shock wave application in the treatment of chronic plantar fasciitis. Foot Ankle Int 2006;27:943–7.
[29] Moghtaderi A, Khosrawi S, Dehghan F. Extracorporeal shock wave therapy of gastroc-soleus trigger points in patients with plantar fasciitis: a randomized, placebo-controlled trial. Adv Biomed Res 2014;3:99.
[30] Rompe JD, Meurer A, Nafe B, et al. Repetitive low-energy shock wave application without local anesthesia is more efficient than repetitive low- energy shock wave application with local anesthesia in the treatment of chronic plantar fasciitis. J Orthop Res 2005;23:931–41.
[31] Tornese D, Mattei E, Lucchesi G, et al. Comparison of two extracorporeal shock wave therapy techniques for the treatment of painful subcalcaneal spur. A randomized controlled study. Clin Rehabil 2008;22:780–7.
[32] Haake M, Buch M, Schoellner C, et al. Extracorporeal shock wave therapy for plantar fasciitis: randomised controlled multicentre trial. BMJ 2003;327:75.
[33] Kudo P, Dainty K, Clarfield M, et al. Randomized, placebo- controlled, double-blind clinical trial evaluating the treatment of plantar fasciitis with an extracoporeal shockwave therapy (ESWT) device: a North American confirmatory study. J Orthop Res 2006;24:115–23.
[34] Ogden JA, Alvarez RG, Levitt RL, et al. Electrohydraulic high-energy shock-wave treatment for chronic plantar fasciitis. J Bone Joint Surg Am 2004;86-A:2216–28.
[35] Rompe JD, Hopf C, Nafe B, et al. Low-energy extracorporeal shock wave therapy for painful heel: a prospective controlled single-blind study. Arch Orthop Trauma Surg 1996;115:75–9.
[36] Gollwitzer H, Diehl P, von Korff A, et al. Extracorporeal shock wave therapy for chronic painful heel syndrome: a prospective, double blind, randomized trial assessing the efficacy of a new electromagnetic shock wave device. J Foot Ankle Surg 2007;46:348–57.
[37] Gollwitzer H, Saxena A, DiDomenico LA, et al. Clinically relevant effectiveness of focused extracorporeal shock wave therapy in the treatment of chronic plantar fasciitis: a randomized, controlled multicenter study. J Bone Joint Surg Am 2015;97:701–8.
[38] Marks W, Jackiewicz A, Witkowski Z, et al. Extracorporeal shock-wave therapy (ESWT) with a new-generation pneumatic device in the treatment of heel pain. A double blind randomised controlled trial. Acta Orthop Belg 2008;74:98–101.
[39] Rompe JD, Decking J, Schoellner C, et al. Shock wave application for chronic plantar fasciitis in running athletes. A prospective, randomized, placebo-controlled trial. Am J Sports Med 2003;31:268–75.
[40] Speed CA, Nichols D, Wies J, et al. Extracorporeal shock wave therapy for plantar fasciitis. A double blind randomised controlled trial. J Orthop Res 2003;21:937–40.
[41] Gerdesmeyer L, Frey C, Vester J, et al. Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled multicenter study. Am J Sports Med 2008;36:2100–9.
[42] Ibrahim MI, Donatelli RA, Schmitz C, et al. Chronic plantar fasciitis treated with two sessions of radial extracorporeal shock wave therapy. Foot Ankle Int 2010;31:391–7.
[43] Malay DS, Pressman MM, Assili A, et al. Extracorporeal shockwave therapy versus placebo for the treatment of chronic proximal plantar fasciitis: results of a randomized, placebo-controlled, double- blinded, multicenter intervention trial. J Foot Ankle Surg 2006;45: 196–210.
[44] Maier M, Milz S, Wirtz DC, et al. Basic research of applying extracorporeal shockwaves on the musculoskeletal system. An assess- ment of current status. Orthopade 2002;31:667–77.
[45] Maier M, Tischer T, Milz S, et al. Dose-related effects of extracorporeal shock waves on rabbit quadriceps tendon integrity. Arch Orthop Trauma Surg 2002;122:436–41.
[46] Wang CJ, Huang HY, Pai CH. Shock wave-enhanced neovascularization at the tendon-bone junction: an experiment in dogs. J Foot Ankle Surg 2002;41:16–22.
[47] Magosch P, Lichtenberg S, Habermeyer P. Radial shock wave therapy in calcifying tendinitis of the rotator cuff–a prospective study. Z Orthop Ihre Grenzgeb 2003;141:629–36.
[48] Labek G, Auersperg V, Ziernhold M, et al. Influence of local anesthesia and energy level on the clinical outcome of extracorporeal shock wave- treatment of chronic plantar fasciitis. Z Orthop Ihre Grenzgeb 2005;143: 240–6.
[49] Yin MC, Ye J, Yao M, et al. Is extracorporeal shock wave therapy clinical efficacy for relief of chronic, recalcitrant plantar fasciitis? A systematic review and meta-analysis of randomized placebo or active-treatment controlled trials. Arch Phys Med Rehabil 2014;95:1585–93.
[50] Dizon JN, Gonzalez-Suarez C, Zamora MT, et al. Effectiveness of extracorporeal shock wave therapy in chronic plantar fasciitis: a meta- analysis. Am J Phys Med Rehabil 2013;92:606–20.
[51] Zhiyun L, Tao J, Zengwu S. Meta-analysis of high-energy extracorporeal shock wave therapy in recalcitrant plantar fasciitis. Swiss Med Wkly 2013;143:w13825.
[52] Aqil A, Siddiqui MR, Solan M, et al. Extracorporeal shock wave therapy is effective in treating chronic plantar fasciitis: a meta-analysis of RCTs. Clin Orthop Relat Res 2013;471:3645–52.
 Tecar
Tecar Shock Wave
Shock Wave Plasma
Plasma Laser
Laser Tesla
Tesla Nikola
Nikola Kayser
Kayser Fusion
Fusion





